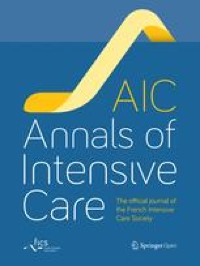
Purpose: Prognostic uncertainty is a major challenge for cancer of unknown primary (CUP). Current models limit a meaningful patient-provider dialogue. We aimed to establish a nomogram for predicting overall survival (OS) in CUP based on robust clinicopathological prognostic factors. Experimental Design: We evaluated 521 patients with CUP at MDACC [MD Anderson Cancer Center, Houston, USA] (2012-2016). Baseline variables were analyzed using Cox-regression and nomogram developed using significant predictors. Predictive accuracy and discriminatory performance were assessed by calibration curves, concordance probability estimate (CPE) ({plus minus}standard error [SE]) and concordance statistic (C-index). The model was subjected to bootstrapping and multi-institutional external validations using two independent CUP cohorts: V1 (MDACC [2017], N=103) and V2 (BC Cancer, Vancouver, Canada and Sarah Cannon Cancer Center/Tennessee Oncology, USA, N=302). Re sults: Baseline characteristics of entire cohort (N=926) included: median age (63 years), women (51%), ECOG-PS 0-1 (64%), adenocarcinomas (52%), {greater than or equal to}3 sites of metastases (30%), median follow-up duration and OS of 40.1 and 14.7 months, respectively. Five independent prognostic factors were identified: gender, ECOG-PS, histology, number of metastatic sites and neutrophil-lymphocyte ratio. The resulting model predicted OS with CPE of 0.69 (SE: {plus minus}0.01) [C-index: 0.71 (95%CI:0.68-0.74)] outperforming Culine/Seve prognostic models (CPE: 0.59{plus minus}0.01). CPE for external validation cohorts V1 and V2 were 0.67 ({plus minus}0.02) and 0.70 ({plus minus}0.01), respectively. Calibration curves for 1-year OS showed strong agreement between nomogram prediction and actual observations in all cohorts. Conclusions: Our user-friendly CUP nomogram integrating commonly available baseline factors provides robust personalized prognostication which can aid cli nical decision making and selection/stratification for clinical trials.